Disclaimer: This article is translated with the assistance of AI.
Denial of Claims: Definition
Denial of claim, as the name suggests, means the insurance company refuses to pay out on a policy claim. It’s a situation no one wants to face, but understanding it can help you navigate the insurance world more smoothly.
Hundreds of Insurance-Related Complaints Annually
According to figures from the Insurance Claims Complaints Committee, in 2019, they received 622 complaint cases, a 4% increase from the previous year. Out of the 361 resolved cases, 89 resulted in compensation totaling HK$6.88 million, with the highest single payout at HK$234,000. However, only 10 cases were successful in claiming, making up just 3% of the complaints. .
Although compared to the nearly 15 million effective long-term business policies or plans in Hong Kong for the whole of 2019, the complaint numbers might seem minor, over 600 cases still add up—it’s worth digging into the reasons behind them to stay informed.
Common Reasons for Denial of Claim
Denial of claim can stem from various reasons; in 2019’s complaint cases, the main one was “policy terms interpretation,” accounting for 37.5% of all cases. This often arises from disagreements on the definition of “medically necessary,” which is one of the most common points of contention.
Another frequent cause is “failure to disclose material facts,” making up 25%, usually because the complainant didn’t fully report their medical history. These two issues—”policy terms interpretation” and “failure to disclose material facts”—have topped the list in complaints received by the Insurance Complaints Bureau from 2015 to 2018.
On top of that, “exclusions” are a common source of disputes. Insurance companies often list pre-existing conditions as exclusions, meaning those conditions aren’t covered. For instance, if an insured person has an issue with their gallbladder, it might be excluded, and later if they claim for liver disease, the company could deny it by arguing it’s related—while the insured might counter that the liver itself isn’t excluded.
These disagreements often boil down to differing definitions of diseases and their triggers. Whether the liver disease is linked to the gallbladder problem requires medical judgment, but it’s smart to carefully review your policy terms—like checking if other diseases stemming from exclusions are clearly listed—to avoid any surprises.
4 Tips to Avoid Denial of Claim
To steer clear of denial of claim situations, keep these 4 tips in mind—they’re your handy toolkit for smoother insurance experiences.
1. Ask Before Claiming
It’s a good idea to check with your insurance company before filing a claim to confirm if the items you’re planning to claim are covered. You could even ask your doctor to estimate the total cost of the procedure, then discuss with the insurer how much they might cover, what you’d have to pay out of pocket, or if the plan can cover the full medical expenses. This way, you can minimize any unexpected gaps.
When applying for compensation, always report accurately, but remember that the entire medical process can affect your claim too—like whether your policy requires a referral from a general practitioner to a specialist, or if your primary doctor is in the insurer’s network (they’re often more familiar with claim procedures and pitfalls).
Plus, for high-cost claims like surgery, it’s wise to get quotes first—seek second opinions from a few doctors and even check online resources for reference. And here’s a tip: while it’s tempting to go for a top-name doctor, if their fees far exceed what’s considered standard, the insurer might deny part or all of it, only covering what they deem reasonable.
2. Prepare Your Documents
Before submitting a claim, gather all necessary documents, such as doctor’s certificates, hospital bills, and the claim form itself. Insurance companies often require any missing items, which can delay your payout.
Additionally, the insurer might investigate the case and ask for authorization to obtain relevant files or information, especially if the claim is soon after policy issuance or if there’s something unclear in the medical records. If the review shows the condition doesn’t meet policy terms, denial could follow.
3. Disclose the Whole Truth When Applying
When applying for insurance, the application form will ask health-related questions, and you must answer truthfully and disclose your full medical history. Don’t hide anything out of fear of higher premiums or rejection—false statements can lead to policy cancellation if discovered.
Sometimes, you might let an insurance intermediary fill out the form or follow their advice on disclosures. If you’re unsure about reporting a health issue, it’s better to disclose it anyway. Always double-check the form before signing, as blaming the intermediary won’t hold up. For example, if you have cataracts but it’s not reported, and you later need to claim for it, the policy might require re-underwriting, potentially adding cataracts as an exclusion and leading to a denied claim.
4. Review Policy Terms and Definitions
Every insurance company’s policy terms and disease definitions vary, so read them carefully before buying. For instance, heart disease is often classified as a “critical illness,” but one company might require at least 90% blockage in two main vessels to qualify, while another might accept 80%.
The truth is, most people—probably 99%—don’t get the full terms until after signing, so they overlook this. That’s why, once you receive your actual policy, take the time to review it during the cooling-off period. If something seems off, contact your intermediary or the insurer right away. During this period, you can cancel and get your premium back if needed.
Bowtie Claims Ratio
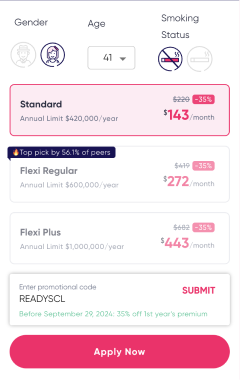
In 2 years, Bowtie has successfully handled multiple claim cases, with a payout ratio as high as 90%. In the claim cases, the ratio of each product* can be referred to the figure below. Press here to learn more about real claim cases.
Among them, there are also cases where claims were not approved, mainly because:
- Not understanding the coverage: For example, in most cases, VHIS only covers inpatient medical expenses; however, customers apply for claims on general outpatient services, so they are not compensated.
- Certain health conditions not declared at the time of claiming: For example, a patient who knew they had hemorrhoids before purchasing insurance did not declare the hemorrhoids condition at the time of purchase, but Bowtie learned of this from medical documents during the claim. After the company re-underwrote based on the hemorrhoids history, it decided that the policy would not cover medical expenses related to hemorrhoids (i.e., excluded items), and the claim case was therefore denied due to “excluded items.”