Disclaimer: This article is translated with the assistance of AI.
What Does an ICD Do?
An Implantable Cardioverter Defibrillator (ICD) is an advanced medical device designed to treat life-threatening arrhythmias, such as ventricular tachycardia and ventricular fibrillation. These arrhythmias can prevent the heart from pumping blood effectively, leading to dizziness, palpitations, shock, or even sudden cardiac death 2,3 .
The heart’s normal beating starts from the sinoatrial node and transmits electrical signals through the heart’s conduction system to various parts, enabling coordinated and regular contractions. However, when issues arise in the conduction system, it may trigger fatal arrhythmias 4 . This is where an ICD plays a crucial role.
The defibrillator mainly consists of a pulse generator and electrode leads, with the leads implanted in the right ventricle and equipped with defibrillation capabilities. When the ICD detects ventricular tachycardia or ventricular fibrillation, it immediately activates treatment by accelerating the pacing rate or delivering an electric shock to restore a normal heartbeat.
Types of ICDs
ICDs are mainly divided into two types: traditional ICDs and subcutaneous ICDs, differing in design, implantation site, and more 1 :
| ICD Type | Traditional ICD | Subcutaneous ICD (S-ICD) |
| Implantation Site | Below the collarbone in the chest, with leads entering the heart | Under the skin on the side of the chest near the armpit, with electrodes extending along the sternum |
| Leads Contact the Heart | Yes | No |
| Functions | Defibrillation + Pacing | Defibrillation only |
| Suitable For | Most arrhythmia patients | Patients with vascular abnormalities, high infection risk, or young patients |
| Size | Smaller | Larger |
When is ICD Surgery Needed?
If a patient has experienced ventricular tachycardia or ventricular fibrillation, these can prevent the heart from pumping blood effectively, leading to shock, fainting, or even cardiac arrest. Implanting an ICD can effectively prevent recurrence of these fatal arrhythmias.
For patients who have survived cardiac arrest, implanting an ICD serves as a preventive measure to reduce the risk of future cardiac arrests.
If a patient’s heart function is severely compromised, such as a left ventricular ejection fraction (LVEF) below 35%, these patients have a higher risk of fatal arrhythmias, and an ICD can effectively prevent sudden cardiac death.
If a patient’s heart rate is too slow (bradycardia), the ICD can act like a pacemaker by sending electrical pulses to help maintain a normal heartbeat. If the heart rate becomes dangerously fast, the ICD delivers a shock to restore normal rhythm.
Some patients, though they haven’t experienced fatal arrhythmias, have abnormalities in the heart’s electrical system or other heart conditions (such as myocardial infarction or dilated cardiomyopathy), putting them at higher risk for ventricular tachycardia or fibrillation. These patients may need an ICD to prevent sudden cardiac death.
For patients who don’t respond well to anti-arrhythmic medications, an ICD provides a more effective treatment option, significantly reducing the risk of sudden cardiac death.
If there’s a family history of sudden cardiac death or genetic testing shows a high risk of arrhythmias, doctors may recommend implanting an ICD to prevent sudden cardiac death.
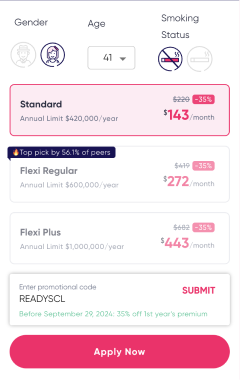
ICD Surgery Costs in Hong Kong
The cost of implantable cardioverter defibrillator (ICD) surgery is relatively high. Package fees generally include pre-operative checks, anesthesia, hospitalization, and other items. It is recommended to consult the hospital in advance and confirm the insurance coverage.
| Hospital | Price |
| Gleneagles Hospital |
|
| Hospital Authority | $30,450 – $37,800 |
ICD Implantation Procedure
The implantable cardioverter defibrillator (ICD) surgery is performed in the hospital’s cardiac catheterization center and takes about 2 to 3 hours. The steps are as follows 4,5,6 :
- Anesthesia: The surgery usually uses local anesthesia, keeping the patient awake. Sedatives may be used if needed to relieve anxiety.
- Pre-operative Monitoring: Nurses will attach electrode pads to the patient’s chest and fit a blood oxygen monitor and blood pressure cuff to monitor ECG, blood oxygen, and blood pressure.
- Disinfection and Incision: The doctor thoroughly disinfects the left chest wall, injects local anesthetic, and then makes an incision of about 3 to 5 cm.
- Contrast Agent and Venipuncture: Contrast agent is injected into the left arm vein, and the subclavian vein is punctured through the left chest wall.
- Electrode Lead Implantation: Under X-ray guidance, the electrode lead is inserted through the subclavian vein into the appropriate position in the heart.
- Pulse Generator Placement: The pulse generator is connected to the electrode lead and placed under the skin or muscle.
- Function Testing: The doctor fully tests the defibrillator’s pacing and defibrillation functions to ensure normal operation.
- Wound Closure: After the surgery, the incision is sutured and covered with dressing.
After the surgery, the patient needs close observation to ensure no abnormalities.
Risks and Side Effects of ICD Surgery
Although ICD implantation is a minor surgery with low risks, complications can still occur. The risks and side effects are as follows 2,4 :
- Wound Infection or Inflammation: The surgical site may become infected, requiring proper care and antibiotic treatment.
- Minor Bleeding or Hematoma: The wound may have minor oozing or blood clot accumulation, which usually resolves on its own.
- Pneumothorax or Hemothorax: During surgery, the lung or blood vessel may be accidentally punctured, leading to pneumothorax or hemothorax, with an incidence rate of less than 1%.
- Cardiac or Pulmonary Wall Perforation: In very rare cases, the surgery may cause perforation of the heart or lung wall, with a risk of less than 0.1%.
- Contrast Agent Allergy: Some patients may have an allergic reaction to the contrast agent, which in severe cases could lead to anaphylactic shock.
- Vascular Damage or Blockage: The surgery may cause vascular damage or blood clot blockage in the vein, with an incidence rate of less than 1%.
- Electrode Lead Displacement or Fracture: The implanted electrode lead may displace or fracture, affecting the defibrillator’s function.
- Pulse Generator Erosion Through Skin: In extremely rare cases, the pulse generator may erode through the skin, requiring further treatment.
- Arrhythmia : The surgery may trigger temporary or persistent arrhythmia.
Additionally, ICD implantation carries a mortality risk of less than 1%. Nevertheless, deaths caused by ICD implantation are extremely rare.
Preparing for ICD Implantation Surgery
Before undergoing implantable cardioverter-defibrillator (ICD) surgery, follow your doctor’s instructions carefully. This includes the following preparations:
- Pre-Surgery Assessment and Tests: Your doctor will arrange an ECG, blood tests, chest X-ray, and more to evaluate surgical risks.
- Signing the Consent Form: The doctor will explain the procedure, its purpose, and risks in detail; you’ll need to sign the consent form.
- Stopping Certain Medications: If you’re on blood thinners, metformin, or anti-arrhythmic drugs, stop them as per your doctor’s advice.
- Inform About Allergies: Tell your doctor about any drug or food allergies beforehand; steroids may be given pre-surgery if needed.
- Fasting Before Surgery: Fast for 4 to 6 hours prior; IV fluids may be administered if necessary.
- Shaving Body Hair: To prevent infection, nurses may shave hair from the surgical site.
- Pregnancy Check for Women: Female patients should provide their last menstrual period date and confirm they’re not pregnant, as radiation could affect the fetus.
- Pre-Surgery Sedation: If needed, your doctor may provide mild sedatives to ease anxiety.
ICD Surgery Aftercare Essentials
After surgery, you’ll need bed rest for a few hours while nurses monitor your blood pressure, pulse, and wound. Most patients are discharged within 1 to 2 days. Key post-surgery precautions include:
- Keep the Wound Clean: The wound will be covered with sterile gauze before discharge; avoid getting it wet and replace if it becomes soaked.
- Showering Tips: You can shower starting on day 7 post-surgery, but avoid direct water on the wound.
- Avoid Strenuous Activity: For the first month, don’t raise the affected arm high or engage in intense exercise to prevent wound reopening or bleeding.
- Regular Follow-Ups: Attend check-ups as scheduled to test the ICD’s function and review recorded data.
- Carry Proof Documents: Always carry your ICD implantation certificate for emergencies.
- Avoid Electromagnetic Interference: Keep your phone at least 15 cm from the ICD and stay away from strong electromagnetic fields (like generators).
- Monitor Wound Condition: If the wound shows redness, swelling, oozing, or inflammation, seek medical attention immediately.
- Watch for Unusual Symptoms: If you experience fainting, chest pain, shortness of breath, or ICD shocks, contact your doctor or go to the ER right away.
- Battery Replacement: ICD batteries last about 3 to 6 years; when depleted, surgery is needed to replace the pulse generator.
- Medication Adherence: Take prescribed antibiotics and pain relievers to prevent infection and ease discomfort.
- Resuming Daily Activities: Discuss with your doctor before gradually returning to normal life, including exercise and hobbies.
- Precautions for Medical Procedures: Inform your doctor ahead of time for checks like MRI to assess risks.
- 1 “Implantable Cardioverter-Defibrillators (ICDs).” Mayo Clinic, 2017
- 2 “Implantable Cardioverter-Defibrillator.” Hong Kong Cardiac Centre, 13 Sept. 2021
- 3 “Defibrillator (ICD) Implantation.” Gleneagles Hospital, 2019
- 4 醫療程序須知沒- 植入式心臟復律除顫器. 聖保祿醫院, 2022
- 5 “心臟起搏器/ 心臟除顫器.” 養和心臟科中心
- 6 “Implantable Cardioverter-Defibrillator (ICD).” Centre Medical, 19 Mar. 2024