Disclaimer: This article is translated with the assistance of AI.
What is Pleural Effusion?
Pleural effusion, commonly known as “water on the lungs,” refers to an abnormal buildup of excess fluid in the space between the chest cavity.
When we breathe, our lungs expand and contract. To prevent damage from excessive friction between the lungs and the chest wall, both the outer layer of the lungs and the inner chest wall are covered by thin membranes. Between these two protective layers, there’s about 3 to 15 milliliters of fluid that provides lubrication during each inhale and exhale.
However, if this fluid is absorbed too slowly or produced too quickly, it can accumulate beyond normal levels in the chest cavity, leading to pleural effusion.
Types of Pleural Effusion
Pleural effusion can be divided into (1) transudative pleural effusion and (2) exudative pleural effusion :
| Causes | |
| Transudative Pleural Effusion |
|
| Exudative Pleural Effusion |
|
To more accurately distinguish between transudative and exudative pleural effusion, clinicians use the patient’s serum total protein level as a benchmark. If the protein level in the pleural fluid is below 25g/L, it’s classified as transudative. Conversely, if it’s above 25g/L, it’s considered exudative.
Causes of Pleural Effusion
Depending on the type of pleural effusion, the causes can vary.
Transudative Pleural Effusion:
Exudative Pleural Effusion:
- Pneumonia
- Cancer
- Kidney diseases
- Other inflammations
Other Common Causes of Pleural Effusion Include:
- Smoking or excessive alcohol consumption
- Pulmonary tuberculosis
- Pulmonary embolism
- Chest injuries
- Immune system disorders
- Infections in the chest or abdominal cavity
- Thoracic duct obstruction or rupture
- Long-term exposure to asbestos
Symptoms of Pleural Effusion
Common symptoms of pleural effusion include:
- Rapid breathing or shortness of breath
- Difficulty breathing
- Coughing
- Chest pain, especially during deep breaths
- Fever , or other flu-like symptoms
How to Diagnose Pleural Effusion?
If you suspect you have pleural effusion, your doctor will start with a simple physical exam and use a stethoscope to listen to the airflow in your lungs.
If something seems off in the lungs, the doctor may arrange further tests, such as a thoracentesis to extract pleural tissue for analysis. Other diagnostic methods include imaging tests like X-rays , ultrasounds , and CT scans , which give doctors a clearer view of your chest and lung structure. You might also need a bronchoscopy to thoroughly examine the airway walls and collect tissue or fluid samples for deeper analysis.
Why Elderly Prone to Pleural Effusion?
Many seniors suffer from conditions like pneumonia, cancer, and heart failure, and pleural effusion is a common complication of these “age-related illnesses.”
On top of that, as we age and our bodies slow down, the elderly are especially vulnerable to respiratory issues, raising their risk of pleural effusion and making them a high-risk group. If diagnosed, it can range from mild breathing difficulties, persistent coughing, and severe chest pain to potentially life-threatening respiratory failure or even death – the stakes are high.
How to Treat Pleural Effusion?
If pleural effusion stems from another medical condition, doctors tackle the root cause – like prescribing antibiotics for pneumonia or diuretics for heart failure – to prevent it from worsening.
For severe cases, they might perform a thoracoscopy or thoracentesis to drain the accumulated fluid and relieve symptoms.
Here’s a summary of the 5 main treatment methods for pleural effusion:
| Pleural Effusion Treatment Methods | Treatment Principle |
| Treating the underlying cause | Focus on curing the disease causing the effusion |
| Thoracoscopy / Thoracentesis | Primarily for extracting tissue for testing, but also drains fluid, combining diagnosis and treatment |
| Thoracostomy | Insert a drainage tube into the chest to remove the fluid |
| Pleurodesis | Use medication to stimulate pleural cells to adhere, preventing recurrent effusion |
| Pleurectomy | Remove thickened or calcified pleural fibers to restore normal lung function |
Diet Tips for Pleural Effusion: Key Precautions
As the saying goes, “prevention is better than cure.” Treatment for pleural effusion only temporarily drains the excess fluid, with a risk of recurrence later on. So, those diagnosed with pleural effusion or at high risk should aim to maintain healthy, balanced eating habits, cutting back on sugar, fat, and alcohol, while eating more vegetables, fruits, and lean proteins.
Plus, high salt and sodium can easily cause excess water to build up in the body. That’s why pleural effusion patients are advised to limit daily sodium intake to no more than 2,000 mg—for instance, by using less salt in cooking meals and steering clear of heavily seasoned foods like those loaded with MSG.
Does VHIS Cover Pleural Effusion Exams & Treatments?
Pleural effusion is linked to heart failure, kidney failure, cirrhosis, and even cancer. If you already have it, it might affect underwriting. For early inpatient medical coverage, consider Bowtie Pink VHIS—plus, pleural effusion exams fall under VHIS protection. If the insured gets a written recommendation from the attending/registered doctor for relevant checks, Bowtie Pink VHIS will fully reimburse 1 the related medical costs.
If further treatment is needed after the exam, Bowtie Pink also covers these expenses:
- Ward and meals
- Attending doctor ward round fees
- Surgeon fees
- Anesthetist fees
- Operating theatre fees
- Pre-admission or post-discharge / day surgery outpatient care* (one prior and three after # )
- Miscellaneous expenses
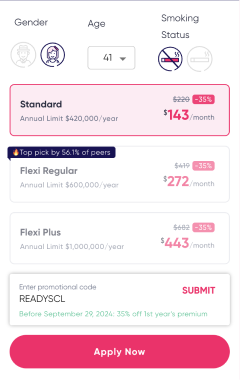
Get a quote for yourself or your family now:
- 1 Full reimbursement means no sub-limit for compensation, and it only applies to specified benefit items. Payable compensation is subject to the remaining deductible (if applicable), annual benefit limit, lifetime benefit limit, and other restrictions including reasonable and customary charges, pre-existing conditions, designated hospital list in Mainland China, and treatment in the United States, etc. For detailed terms and conditions, product risks, and exclusions, please refer to the relevant product website and policy.
- * The Company reserves the right to request proof of the relevant written recommendation, such as a referral letter or statement provided by the attending physician or registered physician in the claim application form.
- # Maximum 1 outpatient or emergency consultation before hospitalization / day surgery; maximum 3 follow-up outpatient consultations within 90 days after discharge / day surgery.
Common Pleural Effusion Questions
Pleural effusion isn’t the same as cancer, but it could be caused by cancer.
When the heart’s ability to pump blood weakens, it raises pressure in the pulmonary veins and capillaries, making it easier for tissue fluid or blood to leak into the lungs, leading to pleural effusion.